You’re Not Crazy, You’re Chronically Dismissed
How to Finally Be Taken Seriously by Doctors
You walk out of the examination room, the heavy door clicking shut behind you, and you feel the familiar sting of tears in your eyes. You waited months for this appointment. You have a list of symptoms that are disrupting your daily life. Yet, you just spent fifteen minutes being told that your pain is likely "just stress," "anxiety," or related to your weight.
You leave with a prescription for antidepressants or advice to "do some yoga," but deep down, you know something physical is wrong.
You are not crazy. You are likely experiencing medical gaslighting.
It is an exhausting, isolating cycle, but it is possible to break it. If you are tired of being ignored, you need a strategy to shift the power dynamic in the exam room. This guide breaks down exactly how to prepare, what to say, and how to finally be taken seriously by doctors so you can get the care you deserve.
What Does It Mean to Be Chronically Dismissed?
Being chronically dismissed in a medical setting—often referred to as medical gaslighting—occurs when a medical professional downplays, invalidates, or ignores a patient's symptoms or concerns.
This is not simply a case of a doctor having a bad day. It is a systemic issue where patients, particularly women, people of color, and those with chronic illnesses, are statistically less likely to receive accurate diagnoses and pain management compared to other groups.
Signs you are being dismissed include:
Interruption: The doctor cuts you off within seconds of you explaining your primary concern.
Attribution errors: All symptoms are immediately blamed on mental health, weight, or hormones without running diagnostic tests.
Minimization: You are told your pain "isn't that bad" or that you are "hypersensitive."
Refusal of testing: The doctor declines to run blood work or imaging despite your persistent symptoms.
Understanding that this is a documented phenomenon, rather than a personal failing, is the first step toward advocating for yourself.
How to Finally Be Taken Seriously by Doctors: 5 Actionable Steps
Hoping for a benevolent doctor is not a strategy. To get results, you must approach your appointment like a project manager. Here is how to advocate for yourself effectively.
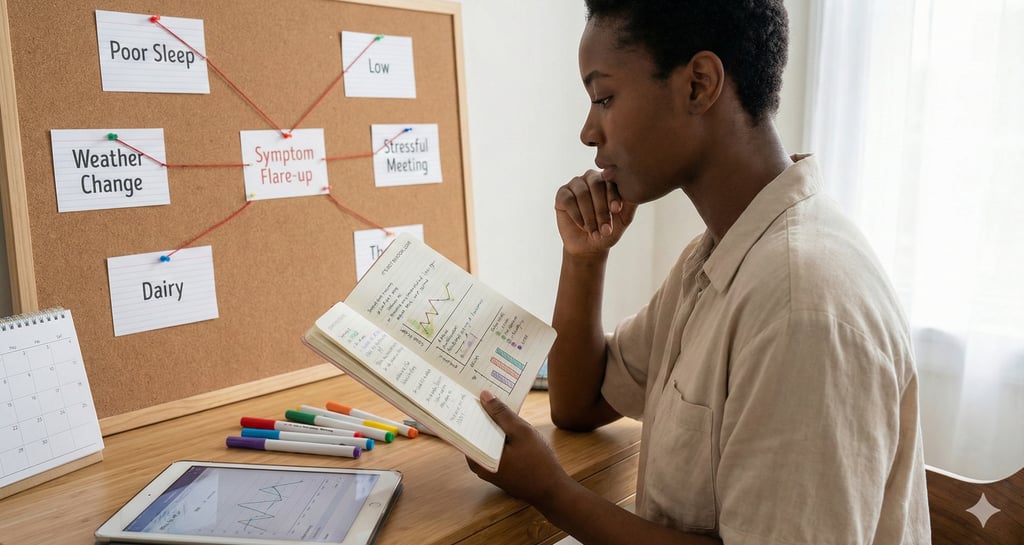
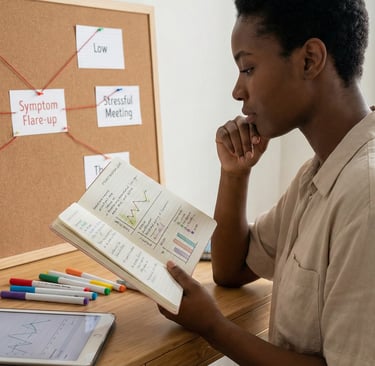
1. Create a Data-Driven Symptom Log
Doctors are trained to look for patterns and data. Subjective statements like "I hurt all the time" are easily dismissed. Concrete data is harder to ignore.
Instead of vague descriptions, bring a printed one-page summary that includes:
Frequency: How many days per week do symptoms occur?
Duration: How long do episodes last?
Triggers: What makes it worse? (e.g., eating certain foods, physical exertion).
Severity: Use a 1-10 scale, but define what a "10" means for you (e.g., "unable to stand").
2. Lead with the "Quality of Life" Impact
Doctors are busy. If you list 20 minor symptoms, they may tune out. Focus immediately on how the symptoms impact your ability to function.
Say this:
"I am here because my fatigue is so severe I can no longer drive my children to school safely." "My joint pain is preventing me from typing, which is threatening my employment."
This frames the issue as a functional disability requiring a solution, rather than a vague complaint.
3. Bring a "Medical Witness"
Whenever possible, bring a partner, friend, or family member to your appointment. This serves two purposes. First, they can take notes while you talk. Second, bias studies show that doctors are often more attentive and thorough when a third party is present in the room. Your witness validates your reality simply by being there.
4. Ask for a Differential Diagnosis
If a doctor suggests a diagnosis that feels dismissive (like "it's just anxiety"), do not just accept it. Ask for a "differential diagnosis."
Ask this:
"I understand you think this might be stress-related. However, what other conditions could mimic these symptoms? What have we ruled out, and what is left on the list?"
This forces the provider to pause and cognitively review other medical possibilities.
5. Use the "Chart It" Technique
This is a powerful tool for accountability. If a doctor refuses to run a specific test you have requested (like an MRI or a thyroid panel), remain calm and make a specific request.
Say this:
"I understand you don't think this test is necessary. Will you please document in my medical chart today that I requested this test and you refused it, along with your reasoning?"
Doctors are legally required to keep accurate records. Often, the realization that their refusal will be permanent record—and potential liability—is enough for them to agree to the test.
Common Mistakes Patients Make (And How to Fix Them)
Even well-prepared patients can fall into traps that undermine their credibility. Avoid these common errors to ensure you are taken seriously by doctors.
Minimizing Your Own Symptoms: Many of us are conditioned to be polite and not be a "burden." When the doctor asks how you are, do not say "I'm okay." Be honest. Say, "I am struggling, which is why I am here."
Overloading the Appointment: Bringing up five different unrelated issues in a 15-minute slot overwhelms the provider. Pick your top two most debilitating symptoms and focus entirely on those.
Getting Emotional: This is unfair, but getting angry or crying can trigger "hysteria" bias in some providers. While your emotions are valid, try to treat the interaction as a business meeting. If you feel overwhelmed, take a deep breath, look at your notes, and stick to the facts.
Drifting Off Topic: Stay focused on your body and your symptoms. Do not spend valuable time discussing personal drama unless it is directly medically relevant.
Practical Tips for Your Next Appointment
Dress the Part: Studies unfortunately suggest that appearance impacts the quality of care. Dressing in "business casual" attire can sometimes signal to a biased provider that you are a professional who expects professional answers.
Send Records Ahead of Time: Do not rely on their office to have your files. Send your symptom summary via the patient portal two days before the visit so it is already in your chart.
Record the Visit: In many regions, you are allowed to record your appointment. Even if you don't record, placing your phone on the table and taking visible notes signals that you are documenting the advice given. Always check your local laws regarding one-party consent before recording audio.
The Benefits of Effective Medical Advocacy
Learning how to finally be taken seriously by doctors is not just about getting a prescription; it is about reclaiming your autonomy.
Practical Benefits:
Faster Diagnosis: Clear communication cuts through the noise, leading to faster testing and answers.
Proper Treatment: When a doctor understands the severity of your condition, you are more likely to get appropriate referrals to specialists.
Paper Trail: Documenting refusals and requests builds a legal and medical history that can help if you need to switch providers later.
Emotional Benefits:
Validation: Knowing you stood up for yourself reduces the feelings of helplessness, even if the appointment wasn't perfect.
Reduced Anxiety: Going in with a plan replaces the fear of the unknown with a sense of control.
[Link to: Internal Link Placeholder - Understanding Autoimmune Flare-Ups] [Link to: Internal Link Placeholder - How to Change Doctors Without Guilt]
You Deserve Answers
You know your body better than anyone else. If you feel something is wrong, trust that instinct. The medical system can be difficult to navigate, but you do not have to do it alone. By preparing your evidence, speaking the language of the medical system, and refusing to accept dismissal, you can get the care you need.
If you are ready to stop leaving appointments in tears and start getting answers, you need the right tools in your hand before you walk through that door.
Download the "Invisible Illness Clarity System" today. This PDF includes a printable symptom tracker, a script for difficult conversations, and a checklist for your next appointment.
